You know what's terrifying? Opening a 500-page medical record only to discover that the nursing notes for days 3 through 7 are identical, word for word. Same vitals. Same assessment. Same "patient stable" language. Except your client coded on day 6.
Welcome to the world of copy-paste documentation, where Electronic Health Records became the enemy of accurate care documentation. And if you're litigating a medical negligence case, these digital ghosts are your new best friend, or your worst nightmare, depending on which side of the courtroom you're standing on.
The Copy-Paste Epidemic: It's Worse Than You Think
Here's the reality: half of all medical records contain duplicative information copied from prior documentation. That's not a typo. Research published in JAMA Network Open confirms what every legal nurse consulting firm already knows, EHR systems made it dangerously easy for providers to clone yesterday's notes into today's chart, regardless of whether the patient's condition actually remained stable.
The problem isn't just sloppy documentation. It's that templated care creates a false narrative of attentive monitoring when the reality might be something far more damaging to the defense's case. When nursing notes look identical despite a patient's deteriorating condition, you're looking at potential evidence of neglect, not continuity of care.

Why Copy-Paste Documentation Is a Legal Smoking Gun
Think about what nursing documentation is supposed to accomplish. It's a real-time chronicle of patient assessment, intervention, and response. When a nurse copies Monday's notes into Tuesday's chart without modification, they're essentially saying, "Nothing changed." But patients aren't static. Conditions evolve. Pain levels fluctuate. Complications emerge.
Copy-paste documentation reveals one of two things:
- The nurse didn't actually assess the patient (which is negligence), or
- The nurse assessed the patient but didn't document changes (which is also negligence, just with better handwriting)
Either scenario is gold for personal injury consulting work. The defense can't argue that the patient received attentive, individualized care when the notes prove otherwise. It's the medical equivalent of claiming you wrote a personalized letter to 50 different people, and then getting caught using mail merge.
The Red Flags: What OnPoint Legal Nurse Consultants Look For
Our medical-legal consulting team doesn't just read charts, we audit them. Here's what separates the pros from the amateurs:
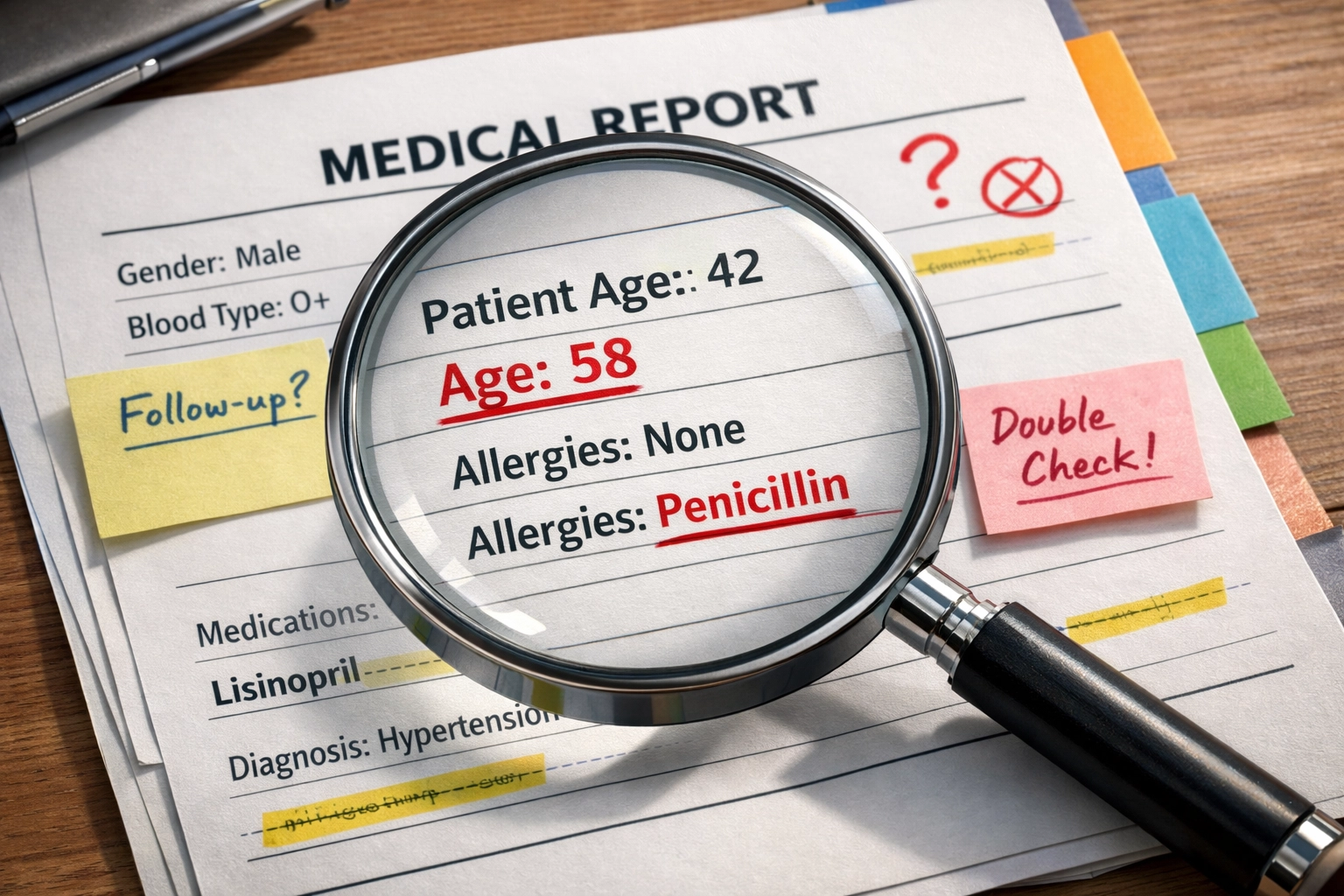
Outdated Information That Won't Die
Ever seen a 56-year-old male patient whose chart includes a history of hysterectomy and C-section? That's not a medical miracle, that's someone who copy-pasted his wife's gynecological history into his record. Yes, that actually happened in documented cases, and it persisted for years.
We scrutinize medication lists that show discontinued drugs, surgical histories that include procedures from five admissions ago, and treatment plans that reference interventions already completed. When information doesn't reconcile with the current clinical picture, that's your first clue that nobody's actually reading what they're documenting.
The "Groundhog Day" Problem
You know something's wrong when day 3, day 4, and day 5 nursing notes are identical down to the timestamp format. Real patient care doesn't replicate like a photocopier. We look for:
- Identical vital signs across multiple shifts (especially suspiciously "normal" ranges)
- Repeated assessment language that doesn't reflect disease progression
- Pain scores that never change despite interventions
- Neurological checks that remain static while the patient's consciousness declines
When the notes suggest stability but the outcome screams deterioration, that gap becomes your narrative. The legal nurse services we provide focus specifically on mapping these contradictions into timelines that juries can understand.

The Inflated "Data Reviewed" Section
Defense loves to point to lengthy progress notes as evidence of thoroughness. But here's the trick: we count how many times the same lab results, imaging studies, or consultant reports appear across different notes. If the attending's note on day 3 lists "reviewed chest X-ray from 1/15," and the hospitalist's note on day 4 lists the exact same thing, and the resident's note on day 5 includes it again: nobody reviewed anything. They all copied the same template.
This inflation tactic makes the record look robust while masking the reality that critical new information (like that deteriorating chest X-ray from day 4) got buried or ignored entirely.
Contradictory Notes That Expose the Lie
Copy-paste documentation often creates internal contradictions because different providers copy from different sources. You'll find notes that say "patient ambulatory" in one section and "patient bedbound" in another. Or a nursing assessment that documents "oriented x3" while physical therapy notes from the same shift describe significant confusion.
These discordant notes aren't just sloppy: they're evidence that no one was synthesizing information or communicating effectively about the patient's actual status. In medical malpractice and elder abuse cases, this fragmentation often precedes catastrophic outcomes.
The Clinical Consequences (That Become Your Legal Arsenal)
Research proves what we see in case after case: copy-paste frequency correlates significantly with patient readmissions within two weeks for the same condition. Translation? When providers rely on templated documentation instead of actual assessment, they miss changes that matter.
Copy-paste errors account for over 36% of documented medical record mistakes. That's more than a third of all charting errors traced directly back to the Control+C/Control+V shortcut. When you're building a negligence case, that statistic transforms from healthcare quality data into litigation ammunition.
High-Risk Documentation Areas: Where to Focus Your Audit
Not all sections of the EHR are equally vulnerable to copy-paste abuse. Our legal nurse consulting firm prioritizes these hot zones:
Medication Reconciliation: This is where copy-paste kills, literally. When medication lists aren't updated, patients receive drugs they shouldn't or miss drugs they need. The chart might show appropriate prescribing, but the reality is that nobody verified what the patient was actually taking.
Problem Lists: These should evolve as diagnoses are confirmed or ruled out. When problem lists remain static despite new clinical information, it suggests nobody's managing the patient's overall care trajectory.
Treatment Plans: Plans should reflect decision-making specific to each visit. When treatment plans are identical across multiple encounters, it indicates a lack of individualized care planning: exactly what you need to prove in negligence cases.
Past Medical History: This should be confirmed and reconciled, not just carried forward. We've seen records where deceased family members remain listed as current contacts because someone copied last year's history without verification.
How OnPoint Digs Deeper Than Software
You might wonder: can't AI or document analysis software catch these patterns? Sure, algorithms can flag duplicative text. But they can't interpret clinical significance. That's where a legal nurse consulting firm with actual nursing expertise becomes indispensable.
We don't just identify copy-paste documentation: we explain what it means. We connect the dots between templated notes on day 4 and the adverse event on day 6. We explain to attorneys and juries why identical nursing assessments across three shifts suggest that nobody actually turned the patient (leading to that pressure ulcer the defense claims was "unavoidable").
Our medical-legal consulting approach combines technical EHR analysis with clinical judgment. We've worked in these systems. We know how the shortcuts happen, where they're most likely to occur, and what they reveal about the actual care delivered: or not delivered.

The Defense's Nightmare: When Copy-Paste Gets Deposed
Here's what makes copy-paste documentation so powerful at trial: it's nearly impossible to defend once exposed. When you show a jury that nursing notes for four consecutive days are identical: down to the punctuation: despite the patient's documented clinical decline, the defense has limited options.
They can't argue the documentation is accurate (because it obviously isn't). They can't claim the patient received individualized care (because the notes prove otherwise). They're left arguing that somehow, despite lazy documentation, the actual care was appropriate: which is a tough sell when the patient ended up dead or permanently injured.
This is where personal injury consulting expertise transforms medical records into courtroom weapons. We create side-by-side comparisons showing the copy-paste patterns. We highlight the timestamps that don't make sense. We identify the exact moment when charting stopped reflecting reality: and connect that moment to when the case went wrong.
Your Next Move
If you're staring at a case where the medical records feel too neat, too consistent, or too damn similar across multiple days or providers, you're probably looking at copy-paste documentation. That's not a documentation quirk: it's potential evidence of substandard care.
The EHR ghost in the machine isn't going away. Healthcare systems have made copy-paste documentation the path of least resistance, and overworked providers take that path constantly. Your job is to catch it before the defense buries it under expert testimony about "standard documentation practices."
That's where OnPoint Legal Nurse Consulting comes in. We audit the digital footprints that others miss. We translate templated documentation into timelines that matter. And we help you build the narrative that turns sloppy charting into liability.
Want us to look at your case? Let's talk about what those suspiciously identical nursing notes are really saying.
